Dementia diagnosis in older adults is not a single test or moment in time. It is a structured clinical process that combines medical history, functional observation, cognitive assessment, and targeted investigations. In geriatrics, evaluation is designed not only to confirm whether dementia is present, but also to identify why cognitive changes are happening and whether any contributing factors are reversible.
In advanced healthcare systems such as Liv Hospital, dementia evaluation is approached as a multidisciplinary investigation that looks beyond memory loss alone and examines the broader picture of aging, physical health, and daily function.
When Cognitive Changes Require Evaluation
Memory lapses are common with aging, but dementia evaluation becomes necessary when cognitive changes begin to interfere with everyday life. Warning signs often include difficulty managing finances, repeating the same questions, getting lost in familiar places, or changes in judgment and personality.
Geriatric assessment focuses on distinguishing normal aging from pathological decline. This distinction is crucial because depression, medication side effects, metabolic disorders, and sensory impairments can all mimic dementia but require very different treatment approaches.
Clinical History: The Foundation of Diagnosis
The evaluation process always begins with a detailed clinical history. Physicians gather information not only from the patient but also from family members or caregivers who observe day-to-day changes.
This stage typically explores:
- onset and progression of cognitive symptoms
- impact on daily activities such as cooking, dressing, and medication use
- behavioral or emotional changes
- medical history including cardiovascular disease, diabetes, or neurological events
- current medications that may affect cognition
Patterns over time often provide stronger diagnostic clues than test scores alone.
Cognitive Assessment Beyond Simple Memory Tests
Cognitive testing is an essential component of diagnosis, but it is used as a guide rather than a definitive answer. Screening tools help estimate severity and identify which cognitive domains are affected.
More comprehensive neuropsychological evaluations may be recommended to assess:
- attention and processing speed
- executive function and problem-solving
- language and comprehension
- visuospatial abilities
- short- and long-term memory
These detailed profiles help clinicians differentiate between Alzheimer’s disease, vascular dementia, Lewy body dementia, and other cognitive disorders.
Medical Evaluation and Reversible Causes
A critical aspect of geriatric dementia diagnosis is ruling out conditions that can be treated. Blood tests and general medical evaluation often reveal contributors such as vitamin deficiencies, thyroid dysfunction, infections, or electrolyte imbalances.
Because older adults frequently live with multiple chronic conditions, careful medical review ensures that symptoms are not being driven by systemic illness rather than neurodegenerative disease.
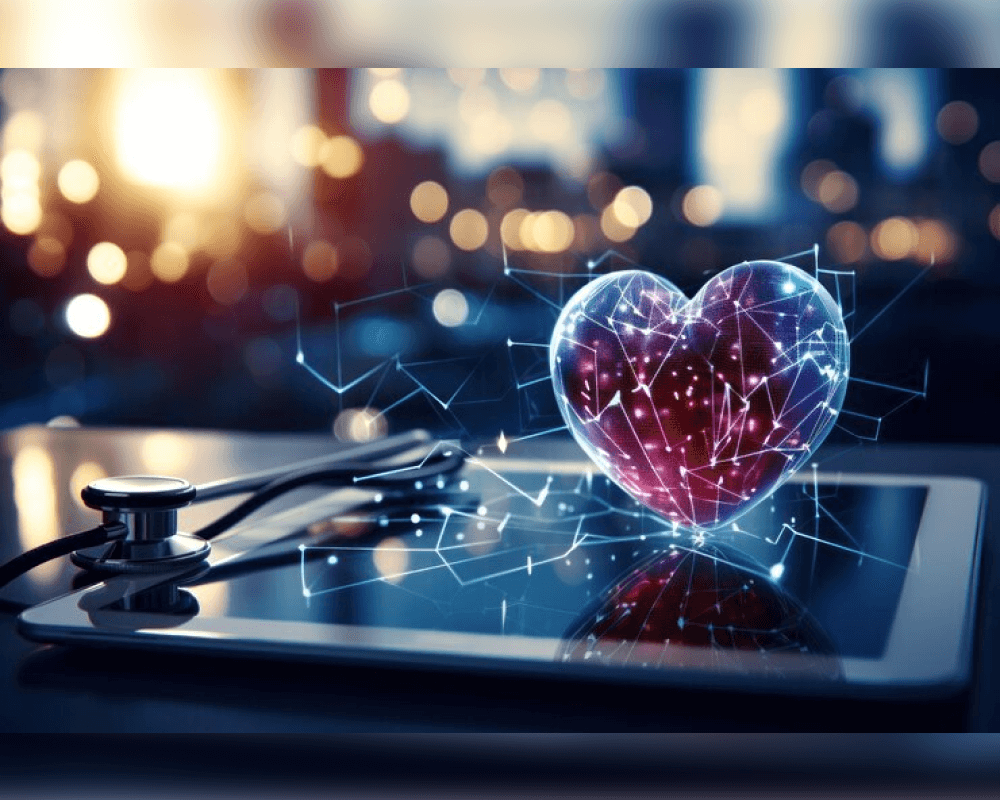
Brain Imaging and Structural Insight
Imaging studies allow clinicians to examine brain structure and identify patterns associated with different dementia types. MRI and CT scans help detect:
- brain atrophy patterns
- evidence of small or large strokes
- tumors or hydrocephalus
- structural changes linked to vascular disease
In selected cases, advanced imaging or biomarker testing may be used to increase diagnostic confidence, particularly when treatment decisions or clinical trial eligibility depend on accuracy.
Functional Assessment: Diagnosis in Real Life
One of the most important aspects of evaluation is understanding how cognition affects real-world function. Dementia is ultimately defined by its impact on independence, not just by test results.
Functional assessment examines:
- ability to manage finances and medications
- safety awareness and fall risk
- personal hygiene and nutrition
- social engagement and communication
This practical evaluation helps guide care planning even before a definitive diagnosis is finalized.
Why a Multidisciplinary Approach Matters
Dementia rarely exists in isolation. Geriatric diagnosis benefits from collaboration between neurologists, geriatricians, psychiatrists, and rehabilitation specialists. This team-based approach ensures that cognitive, emotional, and physical contributors are addressed together.
Within GERIATRICS Dementia Diagnosis and Evaluation, this integrated model improves diagnostic accuracy and allows families to receive clearer guidance about prognosis, treatment options, and next steps.
Diagnosis as the Starting Point, Not the End
Receiving a dementia diagnosis can feel overwhelming, but evaluation is meant to create clarity rather than fear. Accurate diagnosis allows families to plan early, manage risks, and access supportive therapies that preserve quality of life.
For individuals and caregivers who want to complement medical evaluation with everyday strategies for mental clarity, routine, and well-being, lifestyle-focused guidance from platforms like live and feel can help translate clinical insight into sustainable daily habits.