A cataract is often described as “clouding of the lens,” but for many older adults, it feels more like the world has slowly dimmed. Streetlights start to glare, faces look less crisp, and reading becomes tiring even with updated glasses. In geriatric care, cataract treatment is not only about restoring eyesight—it is about protecting independence, confidence, and safety in everyday life.
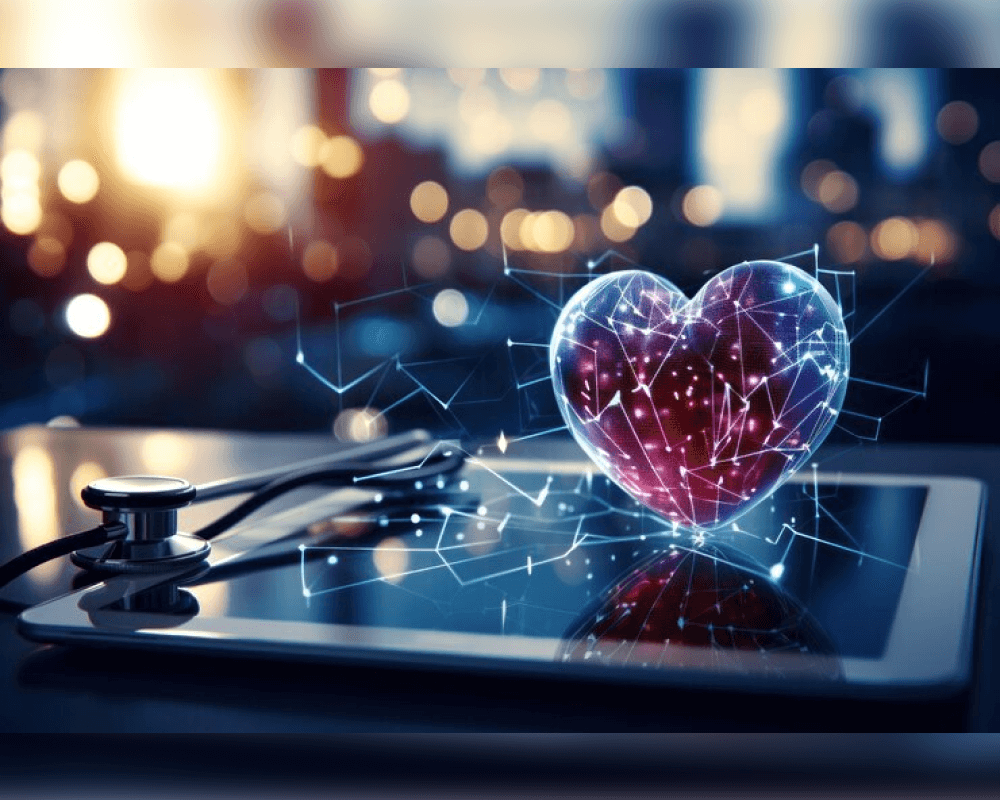
Specialist centers such as Liv Hospital typically approach cataracts within the bigger picture of aging: how vision loss affects balance, driving, medication management, social connection, and fall risk. That broader context shapes how treatment decisions are made and how care is delivered before and after surgery.
When Cataracts Start Interfering With Daily Life
Many people live with early cataracts for years. The tipping point is usually functional, not clinical: the moment vision changes begin to limit normal routines.
Common “quality-of-life” triggers that push cataract care forward include:
- Difficulty driving at night due to halos and glare
- Needing brighter light to read or cook safely
- Trouble recognizing faces at a distance
- Frequent changes in glasses prescription with limited improvement
- Reduced depth perception that makes stairs and curbs riskier
In geriatrics, these symptoms matter because they are strongly linked to falls, fractures, and loss of independence. Cataract care is often framed as preventive functional care—protecting an older adult from avoidable accidents.
Non-Surgical Management: What Actually Helps (and What Doesn’t)
Early on, non-surgical strategies may buy time and improve comfort:
- Lighting upgrades: higher-lumen bulbs, glare-free lamps, task lighting for reading
- Contrast support: bold labels, higher-contrast screens, larger fonts
- Glare control: anti-reflective coatings on glasses, brimmed hats outdoors
- Medication and condition review: controlling diabetes, checking steroid use, and reviewing eye drops that may affect lens clarity
However, cataracts are a structural change in the lens. Once clouding progresses beyond a point, stronger glasses stop making a meaningful difference. That is usually when surgery becomes the most effective treatment.
Cataract Surgery: The Core Treatment in Older Adults
Cataract surgery is widely performed because it directly removes the cloudy lens and replaces it with a clear artificial lens (IOL). But in geriatrics, the decision isn’t simply “Do you have a cataract?” It’s “Is the cataract reducing your safety and ability to live normally?”
A geriatric-focused cataract plan typically considers:
- Overall health and frailty: stamina, mobility, nutritional status, ability to follow post-op instructions
- Medication risks: blood thinners, sedatives, and drugs that affect healing or stability
- Cognitive status: memory issues can affect eye drop schedules and follow-up attendance
- Living environment: stairs, bathroom safety, caregiver support, and transport to appointments
When care is personalized, surgery can improve much more than eyesight—many patients report feeling steadier walking, more confident outside, and less socially withdrawn.
Choosing an Intraocular Lens: Matching Vision Goals to Lifestyle
One reason cataract care feels complex is that lens choices can influence how a person sees after surgery. Older adults often have different priorities than younger patients: predictable vision, safety, reduced glare, and ease with daily tasks.
In practical terms, lens planning usually aims to support:
- Reading and phone use without constant struggle
- Safe navigation indoors and outdoors
- Lower glare sensitivity for night driving or bright daylight
- Reduced dependence on multiple pairs of glasses
A good cataract care discussion connects lens selection to lifestyle: the patient’s typical day, their hobbies, and what “good vision” actually means for them.
Recovery and Aftercare: The Part That Determines Results
Surgery is short; recovery is where outcomes are protected. In geriatric care, aftercare is structured around simplicity and safety.
Post-treatment care commonly focuses on:
- Preventing infection and inflammation with prescribed drops
- Avoiding heavy strain during the first phase of healing
- Monitoring warning signs like worsening pain, sudden vision drop, or increasing redness
- Follow-up scheduling to check healing progress and finalize vision correction
Older adults benefit when aftercare instructions are clear, written, and supported by a family member or caregiver—especially if memory or dexterity is an issue.
Cataract Treatment as “Fall Prevention” and Independence Care
One of the most important geriatric insights is that cataract treatment can reduce downstream risks. Poor vision increases the chance of missing a step, misjudging distances, or avoiding movement altogether. That leads to reduced activity, weaker muscles, and higher fall risk.
So cataract care can be viewed as a functional intervention—restoring the visual cues that help the brain coordinate balance and movement. This is exactly why GERIATRICS Cataract Treatment and Care is not only about the eye, but about the entire daily-life ecosystem of an older adult.
Supporting Eye Health Beyond the Procedure
Even after successful cataract treatment, long-term eye health still matters. The new lens stays clear, but the rest of the eye continues aging, and conditions like glaucoma or macular degeneration can still develop. Consistent check-ups, stable blood sugar control, and healthy habits remain part of senior eye wellness.
If you want practical, non-medical routines that support aging well—sleep, movement, nutrition, and stress habits—resources like live and feel can complement clinical care, especially when the goal is staying active and independent after vision recovery.